Retiree health insurance is changing for PSC retirees. Effective January 1, 2022, the NYC Employee Benefits Program, with the assent of most unions in the Municipal Labor Committee (MLC), is changing the structure of premium-free health insurance available for Medicare-eligible retirees.
They will be transferred to NYC Medicare Advantage Plus (MA+), a private health plan that will manage both Medicare and supplemental benefit payments to providers. The new plan will charge no premium to retirees and is run by the “Alliance,” an amalgam of two companies experienced with serving New York City employees and retirees, EmblemHealth and Empire Blue Cross Blue Shield Retiree Solutions. The latter is part of the national health insurance company, Anthem Health. The Alliance is required to provide the same benefits as traditional Medicare. The initial contract between New York City and the Alliance is for five years.
The PSC sought a delay in the decision to change the structure of city retiree health care, and ultimately voted in the Municipal Labor Committee against the transition to MA+ along with the unions representing doctors and nurses. PSC President James Davis said, “Our members are deeply troubled by the MLC’s rush to vote on this proposal. This austerity measure opens the door to further cost-cutting and diminished benefits in future contracts.”
FALL MAILINGS
The Alliance, in coordination with the New York City Office of Labor Relations (OLR), has sent mailings to Medicare-eligible retirees currently enrolled in Senior Care for their supplemental health coverage describing the new plan and comparing its provisions to Senior Care. (These materials are also on the OLR website.) Retirees enrolled in other supplemental plans should have received mailings in late September. PSC retirees should review the materials carefully. If you are satisfied that the new plan meets your health-care needs, you and the Medicare-eligible dependents currently on your plan will be automatically enrolled in the new Medicare Advantage plan for January 1, 2022. Dependents on your plan who are not Medicare-eligible will continue to be covered by their current insurance plan (usually GHI-CBP). Medicare-eligible spouses must enroll in the same plan as retirees.
However, if you do not wish to be automatically enrolled in the new MA+ plan, you must take action. You must affirmatively “opt out” of the MA+ plan by filling out the opt-out form in the mailing for yourself and a separate opt-out form for any Medicare-eligible dependent. (Your Medicare-eligible spouse or dependent must opt out if you do.) The different ways you can submit the opt-out form are spelled out on the form itself.
If you opt out, your only option is to stay in the plan in which you are currently enrolled, which, starting in 2022, will likely charge a significant monthly premium. For example, Senior Care, in which the vast majority of retirees have been enrolled, will cost $191.57 per month for a retiree starting in 2022 and $383.14 per month for a family (spouse). The 2022 premiums for all plans are available here. PSC retirees do not need to pay for prescription drug coverage in any of the plans because they will continue to be covered by PSC-CUNY Welfare Fund benefits. There is other useful information on the NYC Employee Benefits Program website as well, including benefit comparisons and the MA+ plan description.
Retirees currently in Senior Care who pay for the 365-day hospitalization rider will, if they opt out and remain in Senior Care, continue to be covered by and charged for the rider ($2.83 per month for an individual and $5.66 per month for a family). If you are currently enrolled in Senior Care and are unsure if you are covered by the rider, call EmblemHealth Customer Service at 212-501-4444 and inquire. If you are not covered by the rider and wish to be covered starting in 2022, contact the NYC Employee Benefits Program during November 2021 to sign up. Information about how to do that will be on the PSC-CUNY Welfare Fund and Retiree Chapter web pages. (The rider has not been needed or offered to retirees in other health plans.)
OPT OUT
The decision to opt out requires careful consideration because of cost and access to providers. The only premium-free plans in 2022 will be the NYC MA+ plan, Aetna Medicare Advantage and HIP VIP. (The latter two are only available to those already enrolled in those plans as of December 31, 2021, who opt out of MA+ to stay in them.) Every fall, the NYC Employee Benefits Program will have a retiree health plan annual “transfer period” when retirees can decide to transfer into the MA+ plan or out of it into Senior Care. The other plans will not be available except to those retirees currently enrolled who remain enrolled or those who enroll in MA+ in 2022 and want to switch back to their old plan in 2023.
Some PSC retirees may choose to waive NYC Health Benefits Program coverage altogether and purchase a supplemental “Medigap” health plan on the open market. To do that, instead of the opt-out form, you must waive coverage by completing the NYC Health Benefits Application/Change Form.
However, New York City will continue to reimburse for Medicare Part B and IRMAA only if you are enrolled in a NYC Health Benefits Program health plan. If you waive NYC retiree health plan coverage, you will NOT be eligible for the reimbursement by the city for the Medicare Part B premium (or IRMAA), based on current practice. The PSC is checking into the legality of these reimbursement restrictions. You may re-enroll in city retiree health benefits during the next transfer period.
Take action now to be sure that the NYC Employee Benefits Program has your correct mailing address, particularly if you did not receive a Medicare “Notice of Change” letter from NYC last summer. Submit this form. Also be sure both PSC-CUNY and the Welfare Fund have your correct address by entering your name and correct mailing address, and mailing it to the PSC-CUNY Welfare Fund at 61 Broadway, 15th floor, New York, NY 10006.
PSC ACTION
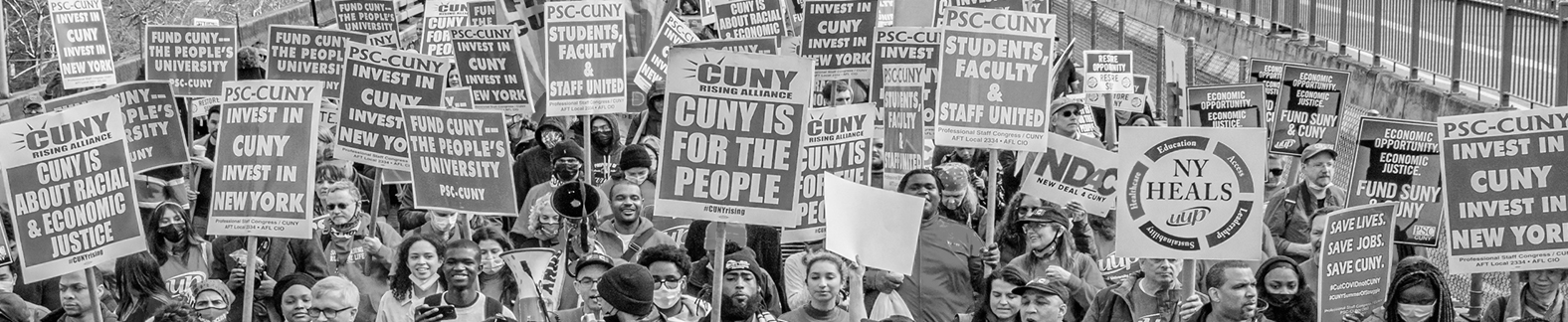
The PSC Retiree Chapter has held a series of meetings about the new plan and the issues and concerns our members have raised. The chapter also organized several protests over the spring and summer urging a delay and greater transparency in the city’s decision-making process. As retiree chapter chair Bill Friedheim has said repeatedly, “Privatizing retiree coverage and shifting the main premium-free NYC retiree health plan away from traditional Medicare with a supplemental plan to a private Medicare Advantage company is a move in the opposite direction from where we should be going, towards a national single-payer program.” The Retiree Chapter web page on the PSC website is an important source of information and the chapter endeavors to keep it as up-to-date as possible.
THE ALLIANCE
Most NYC-area and many national hospitals and doctors are part of the Alliance’s “network.” Retirees can use the Alliance website and click “Find Care” in the middle of the page to find providers in their network.
The Alliance will also cover care provided by providers who accept Medicare rates but are not in its network. However, some retirees’ individual doctors have told their patients they will not participate in a Medicare Advantage plan, even though they may accept Medicare rates. Alliance representatives respond that, because NYC MA+ is an employer-based PPO, not an HMO, providers will not face the same restrictions as with other Medicare Advantage plans. The Alliance has also assured retirees that if the provider still refuses to accept MA+ even after talking to an Alliance “concierge,” the Alliance will reimburse the member for covered treatment at the Medicare rate.
PSC retirees are also concerned about how they will pay premiums if they opt out of NYC MA+. Most NYC retirees belong to a “defined benefit” pension, including PSC retirees who receive pension benefits from TRS or NYCERS. Those retirees will pay premiums out of their monthly pension benefit checks (or deposits). However, the majority of PSC retirees have pensions though TIAA, a defined contribution plan, and CUNY has long required them to maintain a reserve and a lifetime annuity with TIAA to cover retiree health plan expenses. The NYC Office of Labor Relations has assured PSC that they will directly bill TIAA participants whose annuities are insufficient to pay their premium. PSC leaders have been meeting with CUNY and OLR to press for a direct billing option for all TIAA participants who elect to pay premiums, but the reserve and annuity requirements are unlikely to be changed before retirees must make their opt-out decision. The PSC-CUNY Welfare Fund website and PSC Retiree Chapter web page will provide updates.
PSC retirees seeking answers to questions which aren’t answered here, should take these steps in order:
- (1) Check the PSC retirees Medicare Advantage webpage.
- (2) Check the NYC Office of Labor Relations FAQs.
- (3) If they don’t find the answers there, they should call the Alliance toll-free number at 1-833-325-1190, Monday to Friday, 8 am to 9 pm.
- (4) If they still haven’t received accurate answers to their questions, they should check the FAQs on the Welfare Fund website.
- (5) If they don’t find the answers there, only then should they send an email to [email protected].
The decision by the city and the MLC to change PSC retiree health care is frustrating, and has forced retirees to make a difficult and complex decision in a short period of time, in too many cases without adequate information. However, the PSC will continue to fight for our retirees’ rights, by demanding clear information and communicating it promptly.
Deborah Bell is the former executive director of the PSC.